1st Annual Epilepsy Awareness Event & Fund Raiser
Tri County 1k/5k Run, Roll & Stroll has been postponed until December 14th
due to the trajedy of the Mountain fire and the resulting poor air quality. Our hearts go out to all that have suffered terrible losses due to this fire.
Join us for our grand opening ribbon cutting to start the race!
Countdown to Awareness

Let's Talk About Epilepsy
Epilepsy is a complex neurological disorder marked by abnormal electrical activity in the brain, leading to recurrent, unpredictable seizures that can vary greatly in form and severity. While some seizures are brief and may go almost unnoticed, others can cause intense convulsions and loss of consciousness. At Epilepsy Awareness Tri County, we are committed to increasing public awareness and addressing the stigmas often associated with epilepsy. Our resources offer essential information on diagnosing epilepsy, exploring available treatment options, and managing seizures effectively. We also provide guidance on supporting individuals with epilepsy, helping communities become more understanding and inclusive. Together, we can dispel misconceptions and work toward a society that respects and supports everyone living with epilepsy.
Hablemos sobre la Epilepsia
La epilepsia es un trastorno neurológico complejo caracterizado por actividad eléctrica anormal en el cerebro, lo que provoca convulsiones recurrentes e impredecibles que pueden variar significativamente en forma y gravedad. Mientras que algunas convulsiones son breves y pueden pasar casi desapercibidas, otras pueden causar intensas convulsiones y pérdida de conciencia. En Epilepsy Awareness Tri County, estamos comprometidos con aumentar la concienciación pública y abordar los estigmas que a menudo se asocian con la epilepsia. Nuestros recursos ofrecen información esencial sobre el diagnóstico de la epilepsia, las opciones de tratamiento disponibles y la gestión eficaz de las convulsiones. También brindamos orientación sobre cómo apoyar a las personas con epilepsia, ayudando a que las comunidades sean más comprensivas e inclusivas. Juntos, podemos disipar los conceptos erróneos y trabajar hacia una sociedad que respete y apoye a todos los que viven con epilepsia.
Epilepsy is...
Epilepsy is a neurological disorder that disrupts normal brain activity, leading to recurrent, unpredictable seizures. A seizure is a sudden surge of electrical activity in the brain that interrupts regular signal flow, producing symptoms that can range from brief periods of confusion or staring to intense, involuntary jerking movements. Epilepsy can affect individuals of any age, gender, or background, and it is not contagious. With proper treatment and medication, many people with epilepsy can lead full, productive lives. Greater understanding of epilepsy is essential in reducing stigma and fostering support for those impacted by the condition.

La epilepsia es...
La epilepsia es un trastorno neurológico que altera la actividad normal del cerebro, provocando convulsiones recurrentes e impredecibles. Una convulsión es un aumento repentino de actividad eléctrica en el cerebro que interrumpe el flujo regular de señales, generando síntomas que pueden ir desde breves períodos de confusión o mirada fija hasta movimientos bruscos e involuntarios. La epilepsia puede afectar a personas de cualquier edad, género o procedencia, y no es contagiosa. Con el tratamiento y la medicación adecuados, muchas personas con epilepsia pueden llevar vidas plenas y productivas. Una mayor comprensión de la epilepsia es fundamental para reducir el estigma y fomentar el apoyo a quienes se ven afectados por esta condición.
Understand a Seizure When You See One
Understanding seizures is key to demystifying what occurs during these episodes. Seizures, the primary symptom of epilepsy, vary widely in form, depending on which area of the brain is affected and the intensity of electrical activity. A seizure can be compared to a traffic jam in the brain, where the usual orderly flow of electrical signals is disrupted, temporarily halting or redirecting normal processes. This disruption can produce a range of symptoms, from convulsions and altered consciousness to sensory disturbances and unusual behaviors. Much like a traffic jam leads to confusion and unexpected stops, a seizure may cause brief lapses in awareness or involuntary movements. Once the disruption subsides, the brain typically resumes its normal function. Importantly, seizures differ significantly in duration, severity, and presentation, making each person’s experience unique and highlighting the need for individualized diagnosis and management approaches.
Reconozca una Convulsión Cuando la Vea
Es importante saber identificar una convulsión para ofrecer ayuda adecuada cuando ocurra. Una convulsión es un evento provocado por un cambio repentino en la actividad eléctrica del cerebro, y sus manifestaciones pueden variar. Algunas personas pueden experimentar movimientos involuntarios bruscos, pérdida de conciencia o caídas, mientras que otras pueden simplemente quedarse mirando fijamente o parecer confundidas por un breve momento. Comprender estos signos es clave para responder con calma y efectividad. Si observa a alguien con una convulsión, asegúrese de mantener la calma, despejar el área alrededor de la persona para evitar lesiones y evitar restringir sus movimientos. Recuerde que la mayoría de las convulsiones se detienen por sí solas en pocos minutos.
What Triggers a Seizure
Certain factors or triggers can increase the likelihood of seizures in individuals with epilepsy.
Common triggers include:
Emotional stress or anxiety can provoke seizures in some individuals.
Sleep deprivation or irregular sleep patterns may lower the seizure threshold, increasing risk.
Skipping or altering prescribed doses can lead to seizure occurrences.
Excessive alcohol intake or drug use can elevate the likelihood of seizures.
For those with photosensitivity, exposure to flashing lights or patterns can trigger seizures.
High fever, particularly in children, can sometimes lead to febrile seizures.

¿Qué Desencadena una Convulsión?
Claro, aquí tienes un texto en tono autoritario y estilo informativo sobre los desencadenantes comunes de las convulsiones en personas con epilepsia:
El estrés emocional o la ansiedad pueden provocar convulsiones en algunas personas.
La privación de sueño o los patrones de sueño irregulares pueden disminuir el umbral de convulsiones, aumentando el riesgo.
Omitir o alterar las dosis prescritas puede llevar a la aparición de convulsiones.
El consumo excesivo de alcohol o el uso de drogas pueden elevar la probabilidad de convulsiones.
Para aquellos con fotosensibilidad, la exposición a luces intermitentes o patrones puede desencadenar convulsiones.
La fiebre alta, particularmente en niños, puede a veces provocar convulsiones febril.

Types of Seizures
Research is constantly discovering new types of seizures , categories...50 years ago they were known as 1- Petite Mal and 2- Grand Mal. Here are the six main types of seizures, each with distinct characteristics:
Tonic-clonic seizures: These involve a loss of consciousness and violent muscle contractions. They are the type most people picture when they think of seizures.
Absence seizures: These are brief and characterized by a sudden lapse in awareness, often mistaken for daydreaming. They may involve staring into space and subtle body movements, like blinking or lip-smacking.
Myoclonic seizures: These cause sudden, brief jerks or twitches in the muscles, usually without loss of consciousness. They can occur in one part of the body or throughout the entire body.
Atonic seizures: Also known as "drop attacks," these result in a sudden loss of muscle tone, leading to falls or drops.
Tonic seizures: These involve a sudden stiffening of the muscles, often causing the person to fall if they are standing.
Clonic seizures: These cause rhythmic, jerking movements and can sometimes be confused with tonic-clonic seizures if they occur together.
Understanding these different types of seizures helps in their identification and management, allowing for appropriate treatment and support.
Tipos de Convulsiones
Las convulsiones se clasifican en diferentes tipos según su origen y características clínicas. A continuación, se presentan las principales categorías:
Convulsiones tónico-clónicas: Estas convulsiones implican una pérdida de conciencia y contracciones musculares violentas. Son el tipo que la mayoría de las personas imagina cuando piensan en convulsiones.
Convulsiones de ausencia: Se caracterizan por un breve lapso en la conciencia, a menudo confundido con un estado de ensueño. Pueden implicar mirar al espacio y movimientos sutiles del cuerpo, como parpadeo o chuparse los labios.
Convulsiones mioclónicas: Estas causan sacudidas o espasmos musculares repentinos y breves, generalmente sin pérdida de conciencia. Pueden ocurrir en una parte del cuerpo o en todo el cuerpo.
Convulsiones atónicas: También conocidas como "ataques de caída," resultan en una pérdida repentina del tono muscular, lo que provoca caídas o desplomes.
Convulsiones tónicas: Estas implican un endurecimiento repentino de los músculos, lo que a menudo provoca que la persona caiga si está de pie.
Convulsiones clónicas: Causan movimientos rítmicos y espasmódicos y a veces pueden confundirse con las convulsiones tónico-clónicas si ocurren juntas.
Entender estos diferentes tipos de convulsiones ayuda en su identificación y manejo, permitiendo un tratamiento y apoyo adecuados.
Epilepsy Syndromes
Here are some examples of different types of epilepsy syndromes:
Juvenile Myoclonic Epilepsy (JME): This syndrome typically begins in adolescence and is characterized by myoclonic jerks, generalized tonic-clonic seizures, and sometimes absence seizures. These usually occur shortly after waking up.
Lennox-Gastaut Syndrome (LGS): This is a severe form of epilepsy that usually begins in childhood. It involves multiple types of seizures, including tonic and atonic seizures, and is often accompanied by developmental delays and behavioral problems.
Dravet Syndrome: A rare genetic epilepsy syndrome that begins in infancy, characterized by prolonged seizures that are often triggered by fever. Children with Dravet syndrome experience multiple types of seizures and developmental delays.
Childhood Absence Epilepsy (CAE): This syndrome typically starts in early childhood and involves frequent absence seizures, which are brief lapses in awareness that look like daydreaming. Children often outgrow these seizures by adolescence.

Temporal Lobe Epilepsy (TLE): The most common form of focal epilepsy, TLE involves seizures originating from the temporal lobes of the brain. Symptoms can include sensory disturbances, emotional changes, and sometimes altered consciousness.
Rolandic Epilepsy: Also known as benign rolandic epilepsy, this type occurs in children and is characterized by seizures that involve facial twitching, drooling, and speech difficulties. Most children outgrow this form of epilepsy by adolescence.
Síndromes Epilépticos
Aquí hay algunos ejemplos de diferentes tipos de síndromes epilépticos:
Epilepsia Mioclónica Juvenil (EMJ): Este síndrome generalmente comienza en la adolescencia y se caracteriza por sacudidas mioclónicas, convulsiones tónico-clónicas generalizadas y, a veces, convulsiones de ausencia. Estas suelen ocurrir poco después de despertarse.
Síndrome de Lennox-Gastaut (SLG): Esta es una forma severa de epilepsia que generalmente comienza en la infancia. Implica múltiples tipos de convulsiones, incluidas convulsiones tónicas y atónicas, y a menudo se acompaña de retrasos en el desarrollo y problemas de comportamiento.
Síndrome de Dravet: Un síndrome epiléptico genético raro que comienza en la infancia, caracterizado por convulsiones prolongadas que a menudo son desencadenadas por fiebre. Los niños con el síndrome de Dravet experimentan múltiples tipos de convulsiones y retrasos en el desarrollo.
Epilepsia de Ausencia Infantil (EAI): Este síndrome típicamente comienza en la primera infancia e involucra convulsiones de ausencia frecuentes, que son lapsos breves de conciencia que parecen ensoñaciones. Los niños a menudo superan estas convulsiones en la adolescencia.
Epilepsia del Lóbulo Temporal (ELT): La forma más común de epilepsia focal, la ELT implica convulsiones que se originan en los lóbulos temporales del cerebro. Los síntomas pueden incluir alteraciones sensoriales, cambios emocionales y, a veces, alteración de la conciencia.
Epilepsia Rolandica: También conocida como epilepsia rolandica benigna, este tipo ocurre en niños y se caracteriza por convulsiones que involucran espasmos faciales, salivación y dificultades para hablar. La mayoría de los niños superan esta forma de epilepsia en la adolescencia.

8. Surgery and Treatment: While medication can effectively control seizures in about 70% of people with epilepsy, surgical options may be considered for those who do not respond well to medication.
9. Sudden Unexpected Death in Epilepsy (SUDEP): People with epilepsy have a higher risk of sudden unexpected death compared to the general population. The risk is about 1 in 1,000 for adults and 1 in 4,500 for children with epilepsy.
10. Social Impact and Research: People with epilepsy often face stigma and discrimination, which can affect their quality of life. Education and awareness are crucial for reducing stigma and supporting individuals with epilepsy. Ongoing research in genetics, brain imaging, and neurotechnology is improving our understanding of epilepsy and leading to more effective treatments and potential cures.
Hechos y Estadísticas sobre la Epilepsia
Here are ten facts and statistics about epilepsy and seizures:
1. Global Prevalence: Epilepsy affects approximately 50 million people worldwide, making it one of the most common neurological disorders globally.
2. U.S. Prevalence: In the United States, approximately 3.4 million people suffer from epilepsy, affecting individuals across all ages and backgrounds.
3. Seizure Likelihood: About 1 in 10 people will experience a seizure at some point in their life, even if they do not develop epilepsy.
4. Incidence: About 1 in 26 people will develop epilepsy at some point in their lifetime, highlighting the condition's prevalence and impact.
5. Seizure Types: There are more than 40 different types of seizures, each with its own characteristics, symptoms, and treatment approaches.
6. Diagnosis: Epilepsy is typically diagnosed after a person has had at least two unprovoked seizures that were not caused by a known medical condition.
7. Children and Epilepsy: Epilepsy is the most common neurological disorder in children, affecting about 0.5-1% of children worldwide. Many children may outgrow epilepsy by adulthood.
Facts & Statistics About Epilepsy
Hechos y Estadísticas sobre la Epilepsia y las Convulsiones
Prevalencia Global: La epilepsia afecta a aproximadamente 50 millones de personas en todo el mundo, convirtiéndola en uno de los trastornos neurológicos más comunes a nivel global.
Prevalencia en EE. UU.: En los Estados Unidos, aproximadamente 3.4 millones de personas padecen epilepsia, afectando a individuos de todas las edades y antecedentes.
Probabilidad de Convulsiones: Alrededor de 1 de cada 10 personas experimentará una convulsión en algún momento de su vida, incluso si no desarrollan epilepsia.
Incidencia: Aproximadamente 1 de cada 26 personas desarrollará epilepsia en algún momento de su vida, lo que destaca la prevalencia e impacto de esta condición.
Tipos de Convulsiones: Existen más de 40 tipos diferentes de convulsiones, cada una con sus propias características, síntomas y enfoques de tratamiento.
Diagnóstico: La epilepsia se diagnostica típicamente después de que una persona ha tenido al menos dos convulsiones no provocadas que no fueron causadas por una condición médica conocida.
Niños y Epilepsia: La epilepsia es el trastorno neurológico más común en los niños, afectando aproximadamente al 0.5-1% de los niños en todo el mundo. Muchos niños pueden superar la epilepsia al llegar a la adultez.
Cirugía y Tratamiento: Si bien los medicamentos pueden controlar efectivamente las convulsiones en aproximadamente el 70% de las personas con epilepsia, las opciones quirúrgicas pueden considerarse para aquellos que no responden bien a la medicación.
Muerte Súbita Inesperada en Epilepsia (SUDEP): Las personas con epilepsia tienen un mayor riesgo de muerte súbita inesperada en comparación con la población general. El riesgo es de aproximadamente 1 en 1,000 para adultos y 1 en 4,500 para niños con epilepsia.
Impacto Social e Investigación: Las personas con epilepsia a menudo enfrentan estigmas y discriminación, lo que puede afectar su calidad de vida. La educación y la concienciación son cruciales para reducir el estigma y apoyar a las personas con epilepsia. La investigación continua en genética, imágenes cerebrales y neurotecnología está mejorando nuestra comprensión de la epilepsia y conduciendo a tratamientos más efectivos y posibles curas.
What Causes Seizures and Epilepsy
Here are some different causes of epilepsy and seizures:
1. Genetic Factors: Some types of epilepsy run in families, suggesting a genetic link. Mutations in certain genes can increase the risk of developing epilepsy.
2. Brain Injury: Traumatic brain injuries, such as those from car accidents or falls, can lead to epilepsy. Seizures may develop soon after the injury or years later.
3. Infections: Infections like meningitis, encephalitis, and HIV can cause inflammation in the brain, leading to seizures.
4. Stroke: A stroke can damage brain tissue and disrupt normal electrical activity, potentially leading to seizures.
5. Tumors: Brain tumors, whether cancerous or benign, can press on brain tissue and cause seizures.
6. Developmental Disorders: Conditions such as autism and neurofibromatosis are associated with a higher risk of epilepsy.
7. Prenatal Injuries: Brain damage occurring before birth due to infection, poor nutrition, or oxygen deprivation can lead to epilepsy.
8. Metabolic Disorders: Imbalances in body chemistry, such as low blood sugar or electrolyte imbalances, can trigger seizures.
9. Alcohol or Drug Withdrawal: Abruptly stopping alcohol or certain drugs can lead to seizures, particularly in those with dependency issues.
It's important to note that not everyone who experiences seizures has epilepsy. Seizures can be triggered by temporary conditions such as high fever (febrile seizures), electrolyte imbalances, or certain medications. Identifying the underlying cause is essential for proper diagnosis and treatment.
Causas de la Epilepsia y las Convulsiones
La epilepsia es un trastorno neurológico que se caracteriza por la predisposición a sufrir convulsiones recurrentes. Existen diversas causas que pueden contribuir al desarrollo de la epilepsia y las convulsiones:
Factores Genéticos: Algunos tipos de epilepsia tienen un componente familiar, lo que sugiere un vínculo genético. Mutaciones en ciertos genes pueden aumentar el riesgo de desarrollar epilepsia.
Lesiones Cerebrales: Las lesiones traumáticas en el cerebro, como las que ocurren en accidentes automovilísticos o caídas, pueden desencadenar la epilepsia. Las convulsiones pueden aparecer poco después de la lesión o muchos años después.Infecciones: Infecciones como la meningitis, la encefalitis y el VIH pueden provocar inflamación en el cerebro, lo que puede dar lugar a convulsiones.
Accidente Cerebrovascular: Un accidente cerebrovascular puede dañar el tejido cerebral y alterar la actividad eléctrica normal, lo que potencialmente conduce a convulsiones.
Tumores: Los tumores cerebrales, ya sean cancerosos o benignos, pueden ejercer presión sobre el tejido cerebral y causar convulsiones.
Trastornos del Desarrollo: Condiciones como el autismo y la neurofibromatosis están asociadas con un mayor riesgo de epilepsia.
Lesiones Prenatales: El daño cerebral que ocurre antes del nacimiento, debido a infecciones, mala nutrición o privación de oxígeno, puede llevar a la epilepsia.
Trastornos Metabólicos: Desequilibrios en la química del cuerpo, como hipoglucemia o desequilibrios electrolíticos, pueden desencadenar convulsiones.
Síndrome de Abstinencia de Alcohol o Drogas: La interrupción abrupta del consumo de alcohol o ciertas drogas puede provocar convulsiones, especialmente en aquellos con problemas de dependencia.
Es importante destacar que no todas las personas que experimentan convulsiones tienen epilepsia. Las convulsiones pueden ser provocadas por condiciones temporales, como fiebre alta (convulsiones febril), desequilibrios electrolíticos o ciertos medicamentos. Identificar la causa subyacente es esencial para un diagnóstico y tratamiento adecuados.

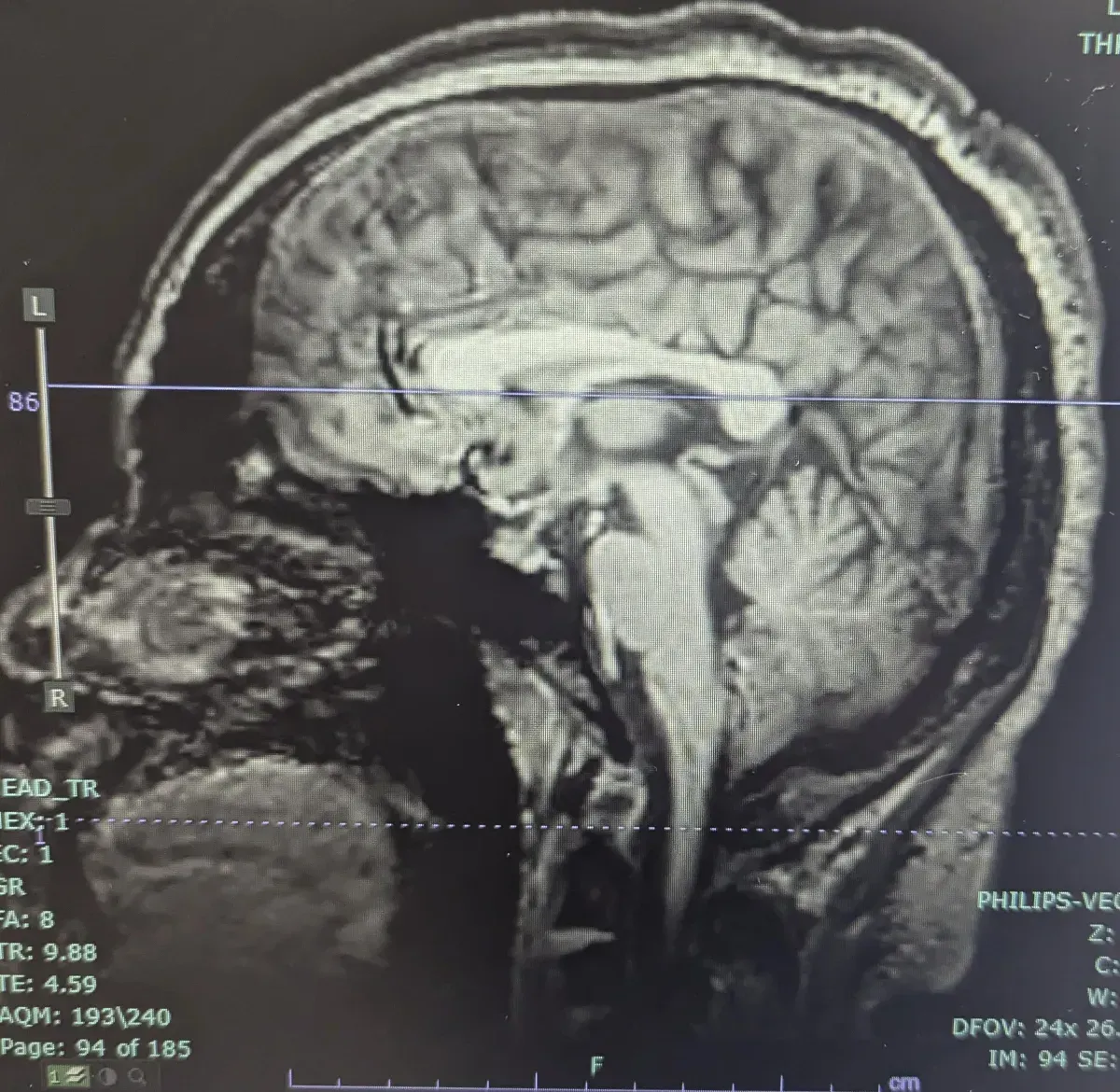
b. MRI (Magnetic Resonance Imaging):
MRI scans provide detailed images of the brain's structure, helping to identify any physical abnormalities or lesions that could be causing seizures.
c. Blood Tests:
These tests can detect metabolic or genetic disorders that may be contributing to seizures.
By combining information from these evaluations and tests, healthcare providers can accurately diagnose epilepsy and develop an effective treatment plan tailored to the individual's needs. Treatment often includes medication to control seizures, lifestyle modifications, and sometimes surgical interventions for those who do not respond to medication. Oftentimes, you need to try several different treatments to find the best suited for each person.
Diagnosing Epilepsy
Diagnosing epilepsy involves a comprehensive evaluation to accurately identify and understand the condition. Here are some of the key methods used:
1. Medical History: Doctors gather a detailed history of seizure episodes, including when they occur, how long they last, and any potential triggers. They also consider family history and any associated symptoms to identify patterns or genetic links.
2. Physical Examination: A thorough neurological examination assesses reflexes, coordination, and sensory function. This helps determine if there are any underlying neurological issues contributing to seizures.
3. Diagnostic Tests:
Several tests are used to diagnose epilepsy and understand its cause:
a. EEG (Electroencephalogram):
This test records electrical activity in the brain and can help detect abnormal patterns that may indicate epilepsy.
Diagnóstico de la Epilepsia
Diagnosticar la epilepsia implica una evaluación integral para identificar y comprender adecuadamente la condición. A continuación se describen algunos de los métodos clave utilizados:
Historia Clínica: Los médicos recopilan un historial detallado de los episodios de convulsiones, incluyendo cuándo ocurren, cuánto duran y cualquier desencadenante potencial. También se considera la historia familiar y los síntomas asociados para identificar patrones o vínculos genéticos.
Examen Físico: Un examen neurológico exhaustivo evalúa los reflejos, la coordinación y la función sensorial. Esto ayuda a determinar si hay problemas neurológicos subyacentes que contribuyan a las convulsiones.
Pruebas Diagnósticas: Se utilizan varias pruebas para diagnosticar la epilepsia y comprender su causa:
a. EEG (Electroencefalograma): Esta prueba registra la actividad eléctrica en el cerebro y puede ayudar a detectar patrones anormales que pueden indicar epilepsia.
b. MRI (Imágenes por Resonancia Magnética): Las exploraciones por MRI proporcionan imágenes detalladas de la estructura del cerebro, ayudando a identificar cualquier anormalidad física o lesión que podría estar causando convulsiones.
c. Análisis de Sangre: Estas pruebas pueden detectar trastornos metabólicos o genéticos que pueden estar contribuyendo a las convulsiones.
Al combinar la información de estas evaluaciones y pruebas, los proveedores de atención médica pueden diagnosticar con precisión la epilepsia y desarrollar un plan de tratamiento efectivo adaptado a las necesidades del individuo. El tratamiento a menudo incluye medicamentos para controlar las convulsiones, modificaciones en el estilo de vida y, a veces, intervenciones quirúrgicas para aquellos que no responden a la medicación. Muchas veces, es necesario probar varios tratamientos diferentes para encontrar el que mejor se adapte a cada persona.
What are some of the challenges?
While epilepsy itself is not typically life-threatening, it can lead to various complications and risks that affect both physical and mental well-being. Understanding these risks can help in managing and mitigating them effectively:
1. Injury: Seizures can cause sudden falls or accidents, leading to injuries such as fractures, cuts, bruises, or head trauma. The unpredictability of seizures makes it important for individuals with epilepsy to take precautions, such as using protective gear or creating a safer living environment to minimize injury risks.
2. Emotional Impact: Living with epilepsy can have a significant impact on mental health. Individuals may experience feelings of anxiety or depression due to the uncertainty of when seizures might occur. Social isolation can also occur if individuals feel embarrassed or fearful of having seizures in public, leading to withdrawal from social activities and relationships.
3. Cognitive Impairment: Some individuals with epilepsy may experience cognitive challenges, such as memory problems, difficulty concentrating, or learning disabilities. These issues can be related to the underlying neurological condition or as a side effect of medication used to control seizures.
4. Status Epilepticus:
This is a serious condition where a person experiences prolonged or continuous seizures lasting more than five minutes or multiple seizures without regaining consciousness in between. Status epilepticus is a medical emergency and can be life-threatening, requiring immediate medical intervention to prevent brain damage or other complications.

5. Sudden Unexpected Death in Epilepsy (SUDEP):
Although rare, SUDEP refers to the sudden, unexplained death of a person with epilepsy. The exact cause is not well understood, but it is more common in individuals with uncontrolled or frequent seizures. Reducing seizure frequency through proper treatment can help lower the risk of SUDEP.
By being aware of these potential complications, individuals with epilepsy and their caregivers can work with healthcare providers to develop strategies to minimize risks and improve overall quality of life. Regular monitoring, effective seizure management, and emotional support are key components of comprehensive epilepsy care.
Aquí hay algunos desafíos comunes que enfrentan los propietarios
de pequeñas empresas y emprendedores:
Aunque la epilepsia en sí misma no es típicamente amenazante para la vida, puede conducir a diversas complicaciones y riesgos que afectan tanto el bienestar físico como el mental. Comprender estos riesgos puede ayudar en su manejo y mitigación de manera efectiva:
Lesiones: Las convulsiones pueden causar caídas o accidentes repentinos, lo que lleva a lesiones como fracturas, cortes, moretones o traumatismos craneales. La imprevisibilidad de las convulsiones hace que sea importante que las personas con epilepsia tomen precauciones, como usar equipo de protección o crear un entorno seguro para minimizar los riesgos de lesiones.
Impacto Emocional: Vivir con epilepsia puede tener un impacto significativo en la salud mental. Los individuos pueden experimentar sentimientos de ansiedad o depresión debido a la incertidumbre sobre cuándo pueden ocurrir las convulsiones. También puede producirse aislamiento social si las personas se sienten avergonzadas o temerosas de tener convulsiones en público, lo que lleva a la retirada de actividades sociales y relaciones.
Deterioro Cognitivo: Algunas personas con epilepsia pueden experimentar desafíos cognitivos, como problemas de memoria, dificultad para concentrarse o discapacidades de aprendizaje. Estos problemas pueden estar relacionados con la afección neurológica subyacente o como un efecto secundario de la medicación utilizada para controlar las convulsiones.
Estado Epiléptico: Este es un estado grave en el que una persona experimenta convulsiones prolongadas o continuas que duran más de cinco minutos o múltiples convulsiones sin recuperar la conciencia entre ellas. El estado epiléptico es una emergencia médica y puede ser amenazante para la vida, requiriendo intervención médica inmediata para prevenir daño cerebral u otras complicaciones.
Muerte Súbita Inesperada en Epilepsia (SUDEP): Aunque es rara, la SUDEP se refiere a la muerte súbita y inexplicada de una persona con epilepsia. La causa exacta no se comprende bien, pero es más común en individuos con convulsiones no controladas o frecuentes. Reducir la frecuencia de las convulsiones a través de un tratamiento adecuado puede ayudar a disminuir el riesgo de SUDEP.
Al ser conscientes de estas complicaciones potenciales, las personas con epilepsia y sus cuidadores pueden trabajar con los proveedores de atención médica para desarrollar estrategias que minimicen los riesgos y mejoren la calidad de vida en general. La monitorización regular, el manejo efectivo de las convulsiones y el apoyo emocional son componentes clave de una atención integral de la epilepsia.
(c)2024, Epilepsy Awareness Tricounty,
all rights reserved.

